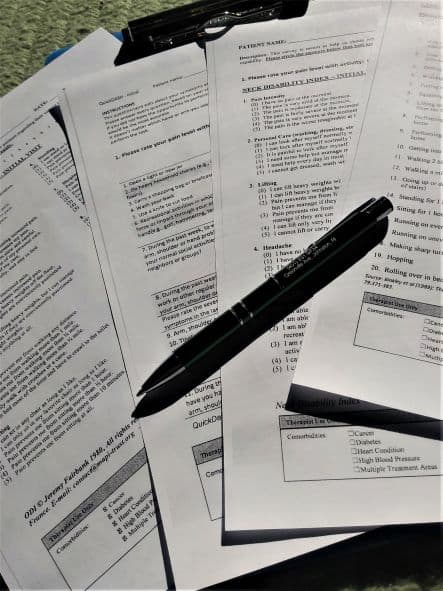
Our patients fill out a functional index at their initial evaluation and reassessments as a measure to gauge their status and their progress. I understand the reason behind this; we like objective measures, and insurance companies like them even more.
But there seems to be so much gray area and variability in how patients approach them. How can this be an accurate representation of a patient’s functional life?
Patient Approaches
I have been practicing for a long time, and I have seen many different perspectives on how the functional indexes are completed.
Too Much or Too Little
Some patients take the index too seriously, while others don’t take it seriously enough.
On one hand, some write notes after each item to explain how they are functioning, and then go on to circle more than one answer. On the other hand, I have seen patients who will, for example, circle the entire “unable” column for every item without even looking at them individually. This can’t possibly be true if they were able to get themselves dressed, leave the house, drive to the clinic, and walk in the door.
Neither way provides an accurate score.
Poor Perception of Dysfunction
Some patients may come in with an unclear vision of their own dysfunction, or they don’t want to complain too much. These folks will then start with a lower percentage of disability, not looking as bad as it truly may be.
After they’ve had some physical therapy and some education, hopefully (if we are doing our jobs right) they will have a more accurate picture of their status and the impact on their life. Their score may then look as if they are getting worse, but in reality, this functional index will represent a more true measure.
Good Days & Bad Days
Patients will fill out these indexes based on how they are feeling in the moment instead of trying to represent an overall functional picture. What if they are feeling relatively good the first time but then are having a different kind of day the next time- a tired day, a stressful day, an inclement weather day? What if that score is all the insurance company considers?
Good days and bad days are part of the healing process. A lower score doesn’t always mean that physical therapy isn’t working. It could mean that they are still very much in need of our services.
What Can We Do?
I understand the concept of statistical significance. I know that the measures we use have been found valid and reliable. But, to me, a person’s daily function is not that black and white.
Hopefully the day will come that our documentation, clinical judgment, and recommendations are enough to justify our services. In the meantime, we need to continue to advocate for our patients. If you receive an insurance decision that you know is not in the patient’s best interest, appeal for what they need. Educate them on the impact honest reporting may have on their care. Talk them through the items when a score does not seem to match the picture you are seeing.
As always, ensure that the rationale for your plan of care is clear and documented. It is the best ammunition you have.

Recent Comments